Scoliosis is a condition that causes curves in your spine. While some curves in the spine are normal, scoliosis causes large curves from side to side. These severe curves can cause pain and breathing issues.
News & Events
- Arthritis
- Back Pain
- Back Surgery
- Collapsed Disc
- Degenerative Disc Disease
- Fibromyalgia
- Herniated Disc
- Max Cohen MD
- Neck Pain
- News
- Osteoporosis
- Physical Therapy
- Pinched Nerve
- Published Articles
- Ruben Torrealba MD
- Sciatica
- Scoliosis
- Spinal Cord Compression
- Spinal Fusion
- Spinal Stenosis
- Spine Injuries
- Spine Injury Prevention
- Spine Tips/FAQS
- Success Stories
- The Surgeon's Perspective
- Whiplash
Michelle Moore – Degenerative spondylolisthesis

Michelle Moore
Martinsville, VA
Degenerative spondylolisthesis
“The surgery helped so much with my pain.”
Michelle Moore traces her initial back problems to the same accident that injured her son Ben in 2004. At the hospital after the accident, doctors told her she had a disc that was bulging slightly. She underwent physical therapy, some injections for pain, and soon was experiencing no problems.
“I exercised, probably weighed a hundred pounds less than I do now, and was doing really good,” she says.
Then, as she drove to a meeting for her job as an administrator for Rockingham County Schools in 2007, a car ran a red light, hit her minivan broadside and sent it careening down an embankment into a power pole. After she was treated and released from the hospital, she continued having pain.
“There was some neck pain, but the majority of the pain was chronic lower back pain, into my hips and my legs,” Michelle says. “But I continued to work because I’m just that type of person. I kept pushing myself.”
She saw an orthopaedist for the continuing pain for much of a year. When nothing helped, he referred Michelle to Max W. Cohen, MD, FAAOS, founder of Spine & Scoliosis Specialists.
“The reason he said he referred me to Dr. Cohen was because I was adamant that I did not want to have back surgery,” Michelle says. He said that Dr. Cohen was a conservative doctor, and he would only suggest surgery if it was the last resort.
Ben Moore – The Surgeon’s Perspective
Ben Moore: Isthmic Spondylolisthesis
Michelle Moore: Degenerative Spondylolisthesis
Max W. Cohen, MD, FAAOS, treated a mother and son, Michelle and Ben Moore, who had different forms of the same condition, spondylolisthesis, which is a slippage of one vertebra onto the other. Spondylolisthesis literally means “vertebra” (spondylo) “to slip” (listhesis) in its Greek origins.
Ben had isthmic spondylolisthesis. Commonly found in adolescent athletes (such as gymnasts, football players and divers), this type of spondylolisthesis occurs after a stress fracture in the area of the vertebra called the pars. The fracture itself is called spondylolysis. Over time, the fractured bone can shift forward. When that happens, it is called spondylolisthesis – and it may or may not cause symptoms.
“There’s a genetic component to this type of spondylolisthesis,” Dr. Cohen says. “The thinnest part of the vertebra is what breaks. That allows the whole vertebral body to shift forward. In most cases, surgery is not necessary for teens with spondylolisthesis.”
“We can treat most cases of spondylolisthesis in kids with a back brace and physical therapy,” Dr. Cohen says. “However, there are some cases where the slippage progresses to the point where surgery is needed. That’s what happened to Ben.”
Ben’s mother, Michelle, had degenerative spondylolisthesis.
“Degenerative spondylolisthesis occurs more in the 40s and 50s age groups,” Dr. Cohen says. “It usually occurs in women, and we’re not sure why that is. It could have something to do with hormonal differences in ligaments.”
In both isthmic and degenerative spondylolisthesis, a shifting of the bone causes the problem.
“But in isthmic (the kind Ben had) the shifting is due to a crack in the pars, so only the front of the bone shifts forward,” says Dr. Cohen. “In degenerative spondylolisthesis, there’s an instability of the entire segment due to degeneration of the joint. The joint is arthritic and incompetent, and the whole bone, front and back, shifts forward.”
“Degenerative spondylolisthesis often occurs along with spinal stenosis, a narrowing of the spinal canal,” Dr. Cohen says.
Spinal fusion is often used to treat both types of spondylolisthesis. Spinal fusion is a complex procedure performed under anesthesia, in which the surgeon joins segments of the spine together. Bone grafts are laid over the vertebra, with splints fashioned from rods, screws and other instrumentation used to hold the grafts in place until they heal. Dr. Cohen has extensive experience with the procedure.
“There are certain disorders of the spine that do well with fusion,” he says. “Spondylolisthesis is one of those.”
Ben Moore – Isthmic Spondylolisthesis

Ben Moore
Martinsville, VA
Isthmic spondylolisthesis
“Now I don’t have any pain. I can just play baseball.”
As a child, Ben Moore was a natural athlete who loved sports. In elementary school and middle school, he played baseball, football and basketball.
But even as he excelled in athletics, a problem was plaguing him. It began at age 11, when he developed back pain after a car he was riding in was rear-ended. After the accident, Ben’s mother, Michelle Moore, took him to a pediatrician, who diagnosed muscle spasms. Over the next four years, Ben developed increasing back pain in everyday life as well as during and after playing the many sports he loved.
“On plays, I’d be diving or sliding, and as I’d get up I would feel this really sharp pain,” he says. “Even when I wasn’t playing, sometimes I would wake up in the morning and get out of bed and there would be a sharp pain in my lower back.”
When his pain continued, Ben’s mother took him to an orthopaedist, who recommended physical therapy and ibuprofen after finding a fracture of a vertebra in his spine.
Ben continued excelling in sports, winning Most Valuable Player and racking up the highest on-base percentage on his 8th grade baseball team.
But the pain persisted. And Ben’s mother continued trying to find help for him, taking him next to a pediatric neurosurgeon who made the same diagnosis and recommendations as the orthopaedist. As Ben’s pain grew worse, he gave up football, then basketball. In 2008, he gave up cross-country after he collapsed at the end of a 5K race.
“I just fell on the ground, I was in so much pain,” he recalls. He worried about whether he would be able to continue the baseball that he loved.
Read The Surgeon’s Perspective
Diagnosis

Ben’s world finally turned around when his mother sought help for her own back problem from Max Cohen, MD, FAAOS, the founding physician of Spine & Scoliosis Specialists in Greensboro. While in the office for an appointment, Michelle saw an article about Dr. Cohen helping another teenager through surgery – and realized he also treated kids. She asked him if he would see Ben.
“I feel like God sent me to Dr. Cohen so Ben could get help,” she says now.
When Ben came for his appointment, Dr. Cohen diagnosed a common adolescent problem: isthmic spondylolisthesis.
“What happens in kids is, there’s a stress fracture of the pars, the thinnest part of the vertebral bone, a condition that is called spondylolysis,” Dr. Cohen says. “Over time, typically in adolescence, the fractured bone can shift forward. When that happens, it is called spondylolisthesis.”
Spondylolisthesis literally means “vertebra” (spondylo) “to slip” (listhesis) in its Greek origins. Isthmic, which refers to the location of the fracture in the pars, is the most common type of spondylolisthesis in adolescents.
“Although Ben traced his onset of pain to a car accident, spondylolisthesis also is a common problem for gymnasts, football players, divers and other athletes who experience fractures from repeated tackles, stress during weightlifting or an overextension of the spine – which later can lead to slippage of the vertebra,” Dr. Cohen says.
Surgery
After Ben’s diagnosis, Dr. Cohen first tried conservative methods, including bracing and physical therapy.
He said, “We’ll try the brace, and we’ll try some exercises and physical therapy again,” Michelle recalls. But he said, “I have to be honest with you. Lots of kids it works for, but in Ben’s case it has gone so long, I don’t think it’s going to work. But we’re going to try it; we’re going to try everything we can before we do surgery.”And they did. “I think we came back six to eight weeks later, and there was no change at all. It was a hard decision for us to have to make, I mean, really hard, but we made the decision to have surgery.”
Just before Christmas 2008, Ben underwent surgery. Michelle delayed surgery for her own back problem, so Ben could get help first.
Dr. Cohen performed a five-hour operation to remove the bone pressing on a nerve in Ben’s spine and fuse Ben’s L5 and S1 vertebrae, using titanium screws and rods. He also inserted a plastic cage between the vertebrae to correct the slippage (spondylolisthesis). The operation took longer than expected due to scar tissue that had formed over the years, encapsulating a nerve and contributing to Ben’s pain.
After the surgery, Dr. Cohen told me,”I don’t know how he ran cross-country. I don’t know how he played baseball. He shouldn’t have even been walking,” recalls Michelle.
Recovery
Ben recovered quickly from the surgery, helped early on by the new Siberian Husky puppy that his parents had given him as a present. Ben named the dog Max after the doctor who got rid of the pain he lived with for years, pain that felt like
“someone was stabbing me with a knife.”
Within two months of his surgery, Ben was doing conditioning with his baseball team and within six months, he had resumed play. In spring 2010, he made the varsity team as a sophomore at Bassett High School. As starting shortstop and second baseman, he helped his high school team become co-champions of Virginia’s Piedmont district. Then, in the summer came his trip to the state finals in Junior American Legion baseball – where his team was runner-up.

Asked in summer 2010 how he felt in comparison to the time before surgery, he says, “On a scale of 1 to 10, I’m a 10 now. Then I was a 2.”
For Ben, a hard-working athlete, the surgery has kept alive his dream. “I want to play college baseball, and if it goes further than that, great,” Ben says.
For his mother, Michelle, the surgery accomplished even more than that.
“Dr. Cohen gave Ben his life back,” she says.
Rick Chaney – The Surgeon’s Perspective
Rick Chaney: Minimally Invasive Lumbar Fusion (also called Minimal Incision Lumbar Fusion)
In the Q and A below, Max W. Cohen, MD, FAAOS, discusses this procedure and how it can help patients.
Q: Your patient Rick Chaney was among the first in the county to have a procedure called a minimally invasive posterior lumbar fusion (or minimal incision spine surgery). What is this?
A: A minimally invasive posterior lumbar fusion is a surgical procedure that allows for a shorter hospital stay, less post-operative pain, a quicker recovery, a smaller risk of infection and a faster return to work than a traditional spinal fusion. It also avoids damage to the paraspinal muscles, which are important for the back to function normally.
Q: I understand you were one of the first surgeons in the country to begin performing this procedure.
A: Yes, I was one of the first to actually do this type of fusion, and I taught other surgeons how to do it from about 2005 through 2008. Today, I don’t do as much training because the procedure is much more common.
Q: What do you do differently with this surgery than with a traditional lumbar fusion?
A: The difference is, with traditional back surgery, we have to cut through muscle as we make an incision in the middle of the spine area. With minimally invasive spine surgery, we make small incisions off to the side of the spine, and then we work in line with the muscle fibers, so we sort of spread the muscle fibers but don’t cut them.
Q: Why is it better if you can avoid cutting the muscle?
A: In the early days of spine surgery, we didn’t worry about the muscle. We just did our work on the spine and then we wondered why many people still had back pain. We know now from MRI scans after surgery that muscle that has been cut develops scar tissue. That’s not good. The muscle is no longer functioning, so that can lead to more pain. We now recognize that the muscle itself is important in the patient’s recovery. So now we pay more attention to preserving the muscle – not only fixing the problem underneath the muscle, but trying to preserve the muscle itself so it is healthy when we are done.
Q: Have studies proven better results long-term for patients who have the minimally invasive procedure?
A: Studies have shown that at least initially patients do better. There’s less blood loss and the hospital stay is shorter. It’s much harder to prove whether the long-term results are better, because there are so many variables between patients, and it’s difficult to prove that patients had comparable, equally bad problems to start with.
Q: Can all fusion patients benefit from this type of surgery?
A: No. It depends on the patient’s individual case. Patients who are having a single-level fusion (where we are fusing only two vertebrae) are the best candidates for the minimally invasive lumbar fusion. However, all patients are benefiting from our increased understanding of the muscle’s importance in recovery. Even in traditional fusions, we are now using techniques that allow us to minimize muscle trauma.
Joyce Cantrell – The Surgeon’s Perspective
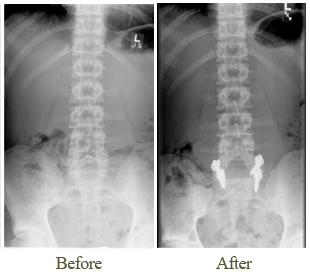
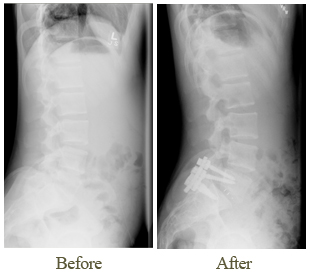
Joyce Cantrell: Adult Scoliosis and Degenerative Disc Disease
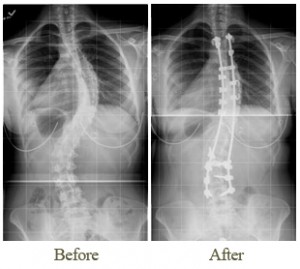
Max W. Cohen, MD, FAAOS, who corrected Joyce Cantrell’s curvature in spinal fusion surgery, notes that adult scoliosis is most common in women – and difficult for many surgeons to treat.
“Most doctors won’t even attempt to tackle a case like this – scoliosis in an adult, an older adult,” Dr. Cohen says. “If the surgeons do something, they often sort of ignore the scoliosis and treat it like a degenerative disc.”
“That is because the great majority of neurosurgeons and orthopedic surgeons were trained to treat only degenerative conditions of the spine,” he says.
“That’s one category of spine surgery,” Dr. Cohen says. “The other category is deformity surgery. That’s where there is some sort of twist of the spine or some sort of curvature. That’s a whole other realm.”
“In a case like Joyce’s, where there’s a deformity – adult scoliosis, or curvature of the spine – in addition to degenerative disc disease, it’s critical to treat both conditions.” Dr. Cohen says. “Many surgeons do not do that.”
“Since very few surgeons have training in deformity surgery, they only see and treat the degenerative problem,” Dr. Cohen Says. “But when you have a degenerative problem superimposed into a scoliosis, ignoring the scoliosis often leads to early failure of the surgery – or it just doesn’t work.”
Dr. Cohen is the only doctor in the Triad with double fellowship training in both types of surgery. He completed a fellowship in spine and scoliosis surgery at Cornell University’s prestigious Hospital for Special Surgery, the top-ranked orthopaedics hospital in the U.S.
The approach to surgery at Spine & Scoliosis Specialists reflects Dr. Cohen’s dual training.
“What we do differently here is we look at the spinal alignment, not just each individual segment, but the whole global alignment and how it affects the patient,” says Dr. Cohen. “When the patient has a disc problem along with scoliosis (an abnormal sideways curvature) or kyphosis (rounding of the back), we feel that you need to address the entire spine – correcting the abnormal alignment in addition to the degenerative disc problem.”
To help Joyce with her scoliosis and degenerative disc disease, Dr. Cohen used instrumentation to fuse her spine from T4 to L4. Because her spinal column had become stiff, Dr. Cohen also performed osteotomies to loosen it up so additional straightening could be obtained.
“And she did very well with that,” he says. “That addressed her scoliosis and the arthritis that had developed within the scoliosis, and it helped her pain.”
Within a couple of years of the surgery, she developed disc degeneration lower on the spine – and had a second surgery for that.
“I was trying originally to save two discs, but with time she had worn those two discs out,” Dr. Cohen says. “So ultimately, we had to extend the fusion down two more. Using innovative techniques, we were able to remove the bottom of the scoliosis surgery and then extend the surgery down across the last two discs in the same kind of fusion we used before. That seems to have been very helpful for her and now she is doing very well.”
He notes that one reason many surgeons don’t perform adult scoliosis surgery is because it is complex surgery that can be especially time-consuming in older patients, with the risk of complications.
“This is surgery that you need to be able to do quickly but precisely,” he says. “We use muscle sparing and minimally invasive techniques wherever we can to minimize surgery time and to improve the recovery. We do so many of these surgeries and have become so adept at it, that we can do them in older adults with successful outcomes and without complications.”
Joyce Cantrell – Adult Scoliosis and Degenerative Disc Disease

Joyce Cantrell
Greensboro, NC
Adult Scoliosis and Degenerative Disc Disease
“I tell everyone Dr. Cohen is a miracle worker.”
Joyce Cantrell suffered from back and joint problems from an early age, just like her sisters, her mother, her grandmother and her great-grandmother before her. But in 1999, when she was in her early 50s, her discomfort moved to a new level.
The excruciating pain she experienced made it difficult for Joyce, a computer teacher in the Bryan School of Business at the University of North Carolina at Greensboro (UNCG), to perform the job she loved.
She began seeing an orthopaedic specialist.
“I went frequently to see him and to get cortisone shots in my back,” she recalls. “Every time I would see him, he would talk very vaguely about how I needed a long-segment fusion. I didn’t know what that was. He would say, ‘I’m afraid you’re going to topple over.'”
But the surgeon was leery of doing the procedure he felt she needed.
He said, “I’m afraid that if I do surgery, you’re going to collapse.” I said, “Well, don’t you think I need surgery then?” and he said,”Well, I’m not going to touch you and risk making your condition worse.”
Meanwhile, Joyce moved to part-time work as a lecturer at UNCG to reduce the stress on her back. “I went part-time because of the pain, because of the terrible pain,” she says. “I couldn’t bend over. I couldn’t pick things up. I could walk, but it was very difficult. Sometimes the pain went down the back of my legs; sometimes my back just hurt. Sometimes I couldn’t walk at all. I used a cane and a walker. You can imagine trying to teach 19-year-olds when you’re in your 50s – not old – using a cane or a walker. I couldn’t pick up my papers if they fell on the floor. The students would have to, and it was really embarrassing.”
By 2003, her pain had worsened, and her orthopaedist said she would need to take frequent rests if she wanted to continue working, even part-time. He said, “Every hour you need to lie down,” Joyce recalls. “So I had a recliner in my office, a full recliner, one that flattens completely out. Every hour on the hour, I’d lie down for about 10 minutes.”
Outside of work, Joyce had to stop doing things she enjoyed – such as driving herself to Raleigh to see her daughter and grandchildren. Even riding in the car that distance caused pain.
In 2005, Joyce’s orthopaedist told her he wanted to refer her to a scoliosis specialist.
“I had no idea I had scoliosis,” Joyce says. “Nobody had told me that.”
The scoliosis specialist was Max W. Cohen, MD, FAAOS, founder of Spine & Scoliosis Specialists, who came to Greensboro in 2002 after completing double fellowship training in spine and scoliosis surgery at Cornell University’s Hospital for Special Surgery, the top-ranked orthopaedics hospital in the country according to U.S. News & World Report.
Read The Surgeon’s Perspective
Diagnosis
When Joyce saw Dr. Cohen, he explained that in addition to degenerative disc disease, she had adult scoliosis, which was causing her spine to curve into an S shape and collapse on itself.
He said,”You are collapsing at something like 10 times the normal rate for a person your age and weight and so forth,” Joyce recalls. “I still didn’t get it.” Then he said,”If we don’t do this surgery for you soon, you will eventually end up in a wheelchair; your spine will collapse,and you won’t be able to breathe.” Dr. Cohen urged her to have surgery as soon as possible. Joyce, who had seen other relatives end up in wheelchairs as a result of similar problems, resigned her job, effective at the end of the school year and began making plans for surgery. But even as she moved forward, she was convinced her life was over.
“I don’t think people understand that pain and fear go together,” she says. “Even though the doctor says, ‘I’m going to fix you,’ you just can’t believe it. I was in so much pain; I thought there was no way out. I had the minister come over to help me pray for courage. I told my kids that life as I knew it was over.”
Surgery
During her surgery in 2005, Dr. Cohen performed a procedure called an osteotomy to break segments of the spine so that it could be straightened. Then, he performed a spinal fusion, using titanium rods and screws to straighten her curved spine and fuse it from T-4 to L-4. Strong pain medication helped her through the first weeks after surgery. Then, gradually she began feeling better as she underwent physical therapy and began resuming normal, everyday tasks. Soon, she was able to get off all pain medications. Within three months, she was driving, and within a year she was back to a normal life.
“Dr. Cohen tells you it takes a year after the surgery, because it really does take a year,” Joyce says.
In 2008, she developed lower back pain due to degenerative disc disease and arthritis. Dr. Cohen performed a second procedure, extending her fusion from L-4 to S-1.
Recovery

Although there are still some things she can’t do, Joyce is amazed at the difference her surgeries made in her life. She enjoys water aerobics several times a week, walks the treadmill at an exercise center, and walks in her neighborhood with her husband. She also enjoys getting in the car and driving to Raleigh to see her grandkids.
“I take no pain medicine now,” she says. “I haven’t taken any pain medicine since 2008. Before surgery I was taking pain medication, but it really did not help. People have said they could see the pain on my face.”
Were it not for the surgery, she is convinced her life would be very different.
“I am certain I would be in a wheelchair by now at the minimum,” Joyce says. “My grandmother and great-grandmother ended up in wheelchairs, and my mother had a back fusion that did not fuse. My sisters have all had back trouble. I have one sister who’s four years older, and she’s had six back surgeries. She’s going to have another one, and I’m very distressed for her. Her doctors evidently were not as good as mine. They did her neck first, and then they fused pieces of her spine. Between the pieces, her back broke. After that, they had to add bridges, and she did not heal correctly.”
Joyce’s advice to others with back and spine problems?
“I have people in my exercise class who are afraid to go to orthopaedic surgeons,” Joyce says. “I tell them to go to Dr. Cohen. I tell everyone Dr. Cohen is a miracle worker. I recommend him to everybody. In fact, I’ve told my sister who’s going to Johns Hopkins for her next surgery to come down here.” I said, “I know Dr. Cohen could fix your back.”
Faye Bunker – Degenerative Disc Disease, with Cervical Spondylotic Myeloradiculopathy and Low Back Pain

Faye Bunker
Greensboro, NC
Degenerative Disc Disease, with Cervical Spondylotic Myeloradiculopathy and Low Back Pain
“I’m totally pain-free for the first time in 10 years.”
Osteoarthritis and degenerative disc disease run in Faye Bunker’s family. Her sister and her younger brother, as well as her late, older brother, all have had multiple back surgeries.
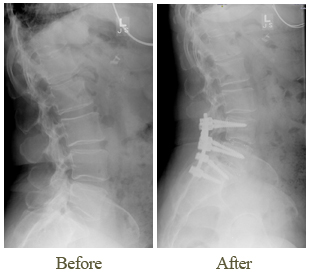
So Faye was not surprised when she began having pain in her lower back and then her knees when she was in her 50s. In 2003, she had both knees replaced. Within a couple years, her back pain had grown worse and she also was having neck pain. She heard popping noises when she turned her neck. Soon, pain began radiating down her left arm.
“I couldn’t lift anything,” she says. “When I was making a gallon of tea, I couldn’t lift it to the shelf in the refrigerator.”
The orthopaedist who had performed her knee replacements referred her to Max W. Cohen, MD, FAAOS, a fellowship-trained spine specialist, for evaluation.
Diagnosis
Dr. Cohen found that Faye had cervical spondylotic myeloradiculopathy (degenerative disc disease with bone spurs and pinched nerves) in her neck. The disc between her C5 and C6 vertebrae was degenerating, and the space between those vertebrae in her neck was narrowing, leading to pinched nerves. He also found degenerating discs in her lower spine, which were causing her chronic lower back pain.
Faye tried conservative treatments, including physical therapy, pain medications and injections, for the pain in her arm and neck but it did not respond. In 2007, Dr. Cohen performed an anterior cervical discectomy and fusion (ACDF), removing the bone spurs and disc that had degenerated and fusing together the surrounding C-5 and C6 vertebrae using bone grafts, a plate and screws.
“I had almost instant relief,” she says.
Then a year later, the pain began again. Imaging studies showed degeneration in an adjacent disc.
“That sometimes happens in patients with degenerative disc disease,” says Dr. Cohen. “All the discs are in a constant state of wear, and we can’t really get ahead of it. We can only fix the main problem we see at that time.”
Faye had a second surgery in 2008 to extend the fusion to C4. That eliminated her neck pain, but she continued to live with constant back pain.
“The back pain was a ‘10′ and it never went away,” she says.
Even though Faye’s back pain was a longstanding complaint, Dr. Cohen had advised doing her neck surgery before even considering back surgery because using a walker – part of the recovery phase of back surgery – would have been difficult with her neck problem. As her back pain grew worse, Faye returned several times to see Dr. Cohen, who advised continuing with conservative, nonsurgical treatments.
Like many doctors, he encourages patients who have degenerative disc disease with chronic lower back pain to exhaust all other treatments before resorting to surgery.
By 2009, Faye’s back pain had become unbearable. Imaging studies showed that the discs between L4 and L5 and L5 and S1 had degenerated.
“I really couldn’t do anything without pain,” she says.
The final straw may have been when she had to give up playing the organ at her church, something she had done for more than 40 years.
“My husband had to help me around, and to get up to my organ, it was two steps,” she says. “I tried everything to make it, but I couldn’t.”
Surgery
Faye returned to Dr. Cohen’s office and asked again about back surgery. Even though she had decided surgery was the answer to her pain, she was a little frightened because her siblings had not fared well.
“My sister had seven back surgeries and none of them worked,” Faye says. “She had one where she went about three months without pain but then she went right back to having pain. My younger brother has had back surgery and it didn’t work – it’s worse now. And I have another brother that has since passed, and he had back surgery, and it didn’t work. So I had a big fear of that, but my pain was so bad, I was willing to take a chance.”
Ultimately, it was her trust in Dr. Cohen that overrode her concerns.
“I had all the confidence in the world in him because of the job he did with my neck,” she says.
In June 2009, Dr. Cohen performed a L4-L5 and L5-L6 transforaminal lumbar interbody fusion with titanium screws in her lower spine. The degenerated discs were removed and a plastic cage was inserted to support the vertebrae. In order to avoid taking bone graft from her hip, synthetic bone grafts were used, along with the cage and screws, to fuse the vertebrae together.
Recovery

The initial recovery period in the hospital after her back surgery was difficult, Faye says.
“For the first few days, you think you have made a mistake,” she says. “You sit there thinking, ‘What have I done?’ You can’t move anything.”
After she was discharged, she was able to use techniques she had been taught in the hospital to lie down and sit up.
“Every day, things got better,” she says.
After several days of physical therapy in her home, Faye says, “I was able to walk with a walker, and then I walked around with a cane for a couple more weeks.”
One of the keys to her recovery was following post-operative instructions to the letter, she says. “I did exactly what the doctor said to do and exactly what the therapist said to do.”
Four months after her surgery, she drove to the beach by herself – following Dr. Cohen’s instructions to stop every hour as she drove.
“It’s been steadily uphill since then as far as getting better,” she says. ” I didn’t have any complications at all and I lay all that to Dr. Cohen. He discusses everything, the pros and cons, and what you have got to do afterwards, and that helps you understand it.”
She believes his advanced training as a spine specialist gives him an edge in helping patients.
“You hear people say, ‘Go to a neurologist if you’ve got back problems instead of an orthopaedic,'” she says. “But I knew Dr. Cohen is a spine specialist and I thought, ‘Well, he should know more about those vertebrae than anybody else.’ And as it turned out, he does.”
Today, Faye says, “I’m totally pain-free for the first time in 10 years.” She once again exercises, does housework, enjoys playing with her great-grandchildren and is back playing the organ three times a week at church. She praises Dr. Cohen for his positive attitude (“He’s got a good personality about him – I just love him”) and his focus on helping patients.
“I ended up at the right place, at the right time, with the right man,” she says with a laugh. “My husband wouldn’t be jealous at all that I said that, because he has his wife back.
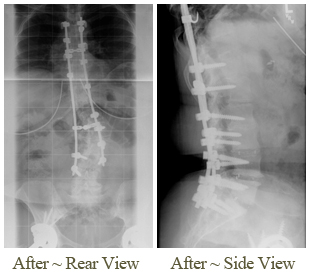
Stephanie Demetrelis – Idiopathic adolescent scoliosis
 Stephanie Demetrelis
Stephanie Demetrelis
Archdale, NC
Idiopathic adolescent scoliosis
“Now I can do what I want and not have to worry about being in pain all the time.”
When Stephanie Demetrelis was 13, she bent over a coffee table at her home – and in that one second, her life changed.
My mom was like,”Oh my goodness, what’s wrong with your back?” Stephanie recalls.
One shoulder blade looked higher than the other, making her appear to have a hump on her back.
Diagnosis
 Stephanie’s mother, Sandra, took her to an orthopaedist, who referred Stephanie to a scoliosis specialist, Max W. Cohen, MD, founder of Spine & Scoliosis Specialists in Greensboro. Dr. Cohen, a fellowship-trained specialist, diagnosed idiopathic adolescent scoliosis, noting a double curve measuring 40 degrees during his initial evaluation in 2003.
Stephanie’s mother, Sandra, took her to an orthopaedist, who referred Stephanie to a scoliosis specialist, Max W. Cohen, MD, founder of Spine & Scoliosis Specialists in Greensboro. Dr. Cohen, a fellowship-trained specialist, diagnosed idiopathic adolescent scoliosis, noting a double curve measuring 40 degrees during his initial evaluation in 2003.
Because Stephanie’s curve was so severe and she was already through most of her growth spurt, she was not a good candidate for a brace – which sometimes can stop further progression during the growth spurt. Instead, Dr. Cohen asked her to return for check-ups at regular intervals to track changes.
“About a year after that, I started having problems with my back,” Stephanie says.
She had been a basketball player when she was younger, but gave that up her freshman year of high school due to pain.
In high school, she took up golf and soon made her school’s golf team. Even as she grew more skilled in that sport, Stephanie was enduring regular pain, and her curvature grew worse – progressing to 46 degrees by 2006.
“If I bent over, you could see this huge hump,” she says. People would say,”Oh, your back.”
Typically, doctors consider surgery when the curvature is 45 or 50 degrees, or if the patient has pain or decompensation (where the head moves out of alignment with the spine). Stephanie and her parents, Sandra and Gary Demetrelis of Archdale, NC, remained hesitant about surgery.
After Stephanie graduated from Vandalia Christian School in 2008, she received a golf scholarship to attend Catawba College in Salisbury, NC. College brought long golf workouts and intensive study sessions, and her discomfort grew worse. The tipping point came in October 2008, when pain caused her to withdraw from a tournament after the first round.
“I was hurting so bad,” she says. I went back to Dr. Cohen and I was like,”I have to get the surgery; I have to get it because I can’t even live a normal life.” Everything I did was so painful.
After returning to Catawba to complete the semester, she had difficulty sitting in class or working on the computer for long periods.
“I remember my last exam, right before Christmas break,” she says. “The exam lasted three hours. It was on the computer, and I was hurting so bad I thought I was going to have to tell the teacher I couldn’t finish. I knew then: I have made the right decision to have surgery.”
Surgery was scheduled for just after the Christmas break and she planned to take the next semester off to recuperate.
“I wasn’t really that scared about it,” Stephanie says. “I felt like Dr. Cohen really knew this was going to help me. I trusted him completely.”
Surgery
 During the surgery on January 6, 2009, Dr. Cohen used a state-of-the-art technique to straighten Stephanie’s curved spine – utilizing screws, hooks, titanium rods and a Dacron band called a universal clamp. Stephanie was the first scoliosis patient in the U.S. to benefit from the clamp, which Dr. Cohen helped develop for U.S. use with Abbott Spine. Bone grafts were then laid over her spine to create a “scaffolding” for the vertebra to grow together in the new straightened position.
During the surgery on January 6, 2009, Dr. Cohen used a state-of-the-art technique to straighten Stephanie’s curved spine – utilizing screws, hooks, titanium rods and a Dacron band called a universal clamp. Stephanie was the first scoliosis patient in the U.S. to benefit from the clamp, which Dr. Cohen helped develop for U.S. use with Abbott Spine. Bone grafts were then laid over her spine to create a “scaffolding” for the vertebra to grow together in the new straightened position.
“We’re actually tricking the body into thinking it has a fracture that needs to heal,” says Dr. Cohen.
Key to the success of the procedure is the “hardware” used to straighten the spine.
It holds the vertebra in place while the bone grafts grow together.
Recovery
 Stephanie spent a week in the hospital, feeling pretty “miserable,” she says, and another month recovering at home before she began feeling a lot better. Gradually, Dr. Cohen allowed more activity, and in July 2009, Stephanie began practicing golf again.
Stephanie spent a week in the hospital, feeling pretty “miserable,” she says, and another month recovering at home before she began feeling a lot better. Gradually, Dr. Cohen allowed more activity, and in July 2009, Stephanie began practicing golf again.
“I wanted to play so bad,” she recalls. “I just could not wait to get back out there.”
Stephanie was elated when, two weeks after she began practicing again, she won the girls’ High Point Junior Golf Championships in her age division.
In fall 2009, she returned to college and the golf team at Catawba College. By spring of 2010, she was finding the rigors of four-hour practices, long tournaments and college too much and decided not to continue in competitive golf.
“I still play but for fun now,” she says.
 In fall 2010, she transferred to the University of North Carolina at Greensboro to major in travel and tourism. She is amazed that she can sit in class or work at a computer for hours without pain.
In fall 2010, she transferred to the University of North Carolina at Greensboro to major in travel and tourism. She is amazed that she can sit in class or work at a computer for hours without pain.
“I used to not be able to study or sit at a computer for long,” she says. “Now I don’t hurt at all when I’m in class or working on the computer. I’m not in any pain.”
Her advice for other young scoliosis patients who are in pain and considering surgery?
“If you have scoliosis and you’re in pain, you need to get the surgery,” she says. “I definitely recommend it.”
The Parts of Your Spine and How They Work
The spine is one of the most important parts of your body. Without it, you could not keep yourself upright or even stand up. Your spine gives your body structure and support. It allows you to move and bend. The spine also protects your spinal cord. The spinal cord is the column of nerves that connects your brain with the rest of your body, allowing you to control your movements. Without a spinal cord, you could not move any part of your body, and your organs could not function. That is why keeping your spine healthy is vital if you want to live an active life.
Vertebrae, Ligaments, Tendons, and Nerves
Your spine is made up of 24 small bones. Each bone is called a vertebra (ver-ta-bruh). These are the building blocks of the spinal column. Together, all the bones that make up the spine are called vertebrae (vert-a-bray).
The vertebrae protect and support the spinal cord, and bear most of the weight put on your spine. Each vertebra is made up of a large bone called the body, and laminae (lam-in-ay) which extend from the body and form a ring to enclose and protect the spinal cord. The laminae includes the spinous (spine-us) process, which is the bone you feel when you run your hand down someone’s back, two transverse (trans-verse) processes where the back muscles connect to the vertebrae, and the pedicle (ped-i-cuhl) that connects the two sides of the lamina.
Between each vertebra is a soft, gel-like cushion called a disc. The disc helps absorb pressure and keeps the bones from rubbing against each other. Each vertebra is held to the others by groups of ligaments. Ligaments connect bones to bones. There are also tendons in the spine which connect muscles to the vertebrae. Like other parts of the body such as the knee or elbow, the spinal column also has joints. Spinal column joints are called facet (fuh-set) joints. Facet joints link the vertebrae together and give them the flexibility to move against each other.
When the vertebrae stack on top of each other, the holes line up to form a long hollow tube that runs the length of the spine. The spinal cord runs through this long hollow tube. The spinal cord itself is a large bundle of millions of nerves that carry messages from your brain to the rest of your body, and from every part of your body back to your brain. The spine branches off into thirty-one pairs of nerve roots. These roots exit the spine on both sides through spaces called neural foramina (noor-al for-a-min-ah) between each vertebra.
Segments of the Spine
The spine itself has three main segments: the cervical (ser-vi-cal) spine, the thoracic (thor-a-sic) spine, and the lumbar (lum-bar) spine. The cervical spine is the upper part of the spine known as the neck. It is made up of seven vertebrae. The thoracic spine is the center part of the spine. It is made up of 12 vertebrae. The lumbar spine is the lower portion of the spine. It is usually made up of five vertebrae, however, some people may have six lumbar vertebrae. Having six vertebrae does not seem to cause a problem.
Below the lumbar spine is the sacrum (sack-rum). The sacrum is actually a group of specialized vertebrae that connects the spine to the pelvis. Before birth, these vertebrae grow together (or fuse) creating one large “specialized” bone that forms the base of your spine and center of your pelvis. The nerves that leave the spine in the sacral region control bowel and bladder functions and give sensation (feeling) to the crotch area.
There are two sacroiliac (sack-row-ill-e-ack) (SI) joints in your pelvis that connect the sacrum to the ilium (ill-e-um) (the large pelvic bone). The SI joints connect your spine to the pelvis, and thus, to the entire lower half of your skeleton.
Like any other joints in your body, there is cartilage on both sides of the SI joint surfaces. But, unlike most other joints, the SI joints are covered by two different kinds of cartilage. The surfaces of the joint where movement occurs have both hyaline (high-a-leen) (which is glassy and slick) and fibrocartilage (figh-bro-cart-il-age) (which is spongy) surfaces that rub against each other. The joints also have many large ridges (bumps) and depressions (dips) in the surface that fit together like a puzzle.
The SI joints are also unique because they are not designed for much motion. It is common for the SI joint to become stiff and actually “lock” as people age. The SI joint only moves about two to four millimeters when bearing your body’s weight and bending forward. This small amount of motion in the joint is described as a “gliding” type of motion. Due to the small amount of movement and the complexity, finding out about the SI joints’ motion is very difficult during a physical exam.
The SI joints are said to be viscoelastic (vis-ko-e-las-tick). This means that the major movement of the joint comes from giving or stretching. This motion is quite different than the hinge motion of the knee or the ball and socket motion of the hip. The SI joints absorb shock for the spine by stretching in various directions. The SI joints may also provide a “self-locking” mechanism that helps you to walk. The joints lock on one side as weight is transferred from one leg to the other.




